Exercises for spinal injuries. Rehabilitation training after a back injury
Injury to the cervical spine involves the use of a wide variety of treatment methods, depending on the duration of the injury, its degree and nature, as well as the severity of neurological disorders.
In the acute period, treatment consists of eliminating the displacement of the vertebrae, decompressing the membranes of the spinal cord and its roots, creating the most favorable conditions for restoring anatomical "relationships", preventing relapses and secondary damage to the nerve elements.
In a longer period of recovery (rehabilitation), an injury to the cervical spine involves the direction of the main efforts to increase the strength and endurance of the muscles of the neck and trunk, and later on to increase the mobility of the spine.
Most often, the most mobile cervical vertebrae - C5-C6 are subject to injury.
Rehabilitation for spinal injuries today cannot be imagined without exercise therapy, not only in the long-term, but also in the acute period. This feature is explained by the fact that exercise therapy performs a variety of functions, including the prevention of the formation of bedsores, reduces the phenomena of general asthenic syndrome, helps prevent thrombosis, and helps to normalize digestion.
In particular, the timely and sufficient duration of the exercise therapy complex for injuries of the cervical spine prevents the addition of such dangerous complications as congestive pneumonia or dysfunction of the pelvic organs.
Injuries of the cervical spine - contraindications to exercise therapy
Contraindications to physiotherapy exercises for injuries of the cervical spine are:
- The general serious condition of the patient.
- Persistent pain syndrome.
- Persistent increase in body temperature (37.5 ° C and above).
- Persistent increase or decrease in blood pressure.
- Progressive increase in neurological symptoms (deterioration of motor activity in the limbs, impaired sensitivity).
- Severe asthenic syndrome in the period immediately after the implementation of the complex of physiotherapy exercises.
Injury of the cervical spine - exercise therapy in conservative therapy. General provisions
Conservative treatment of injuries of the cervical spine begins with traction, which lasts for 2-4 weeks. At the same time, exercise therapy is prescribed on the 2nd-3rd day after the injury in order to prevent possible complications associated with prolonged immobilization.
During this period, the complex of physiotherapy exercises includes elementary general developmental exercises for the distal limbs and breathing exercises (static and dynamic) in a ratio of 1:2 (in the first days), and subsequently - 3:1 and 4:1. Leg movements are performed only in a lightweight version, since raising a straight leg can cause pain due to tension in the back muscles.
15-30 days after the trauma of the cervical spine, traction is replaced with a plaster or plastic semi-corset with a collar (orthopedic collar), which is worn for 8-10 weeks. Since that time, the volume of physiotherapy exercises and their duration have been increasing, the patient's motor regimen has been expanding. He is allowed to sit on the bed with his legs down on a low bench, and then move independently - first within the ward, then around the department.
An injury to the cervical spine during the period of wearing an orthopedic collar (immobilization) “requests” exercise therapy aimed at improving blood circulation in the area of damage in order to stimulate regeneration processes, prevent atrophy of the muscles of the neck, shoulder girdle and upper limbs, as well as strengthen the muscles of the body, restore correct posture and walking skills. Therefore, the complex of physiotherapy exercises includes general strengthening exercises covering all muscle groups performed in the initial position lying, sitting and standing (with support on the back of a chair, bed). Use exercises with light weights, light resistance. Movements (tilts) of the body forward are contraindicated.
To strengthen the muscles of the neck and shoulder girdle, isometric muscle tension is recommended, initially 2-3, then 5-7 seconds. The procedure is performed 3-4 times during the day. The duration of exercise therapy during this period of rehabilitation for injuries of the cervical spine is 15-20 minutes.
After 8-10 weeks after the trauma of the cervical spine, the fixing bandage is removed, and the main efforts of exercise therapy are directed to strengthening the muscles of the neck, shoulder girdle and upper limbs, restoring movements in the cervical spine.
In the first days after the termination of immobilization, to eliminate the additional vertical load on the cervical spine, classes are carried out only in the initial position lying down, then sitting and standing.
Injuries of the cervical spine at the end of the immobilization period suggest the introduction of isometric tension in the muscles of the neck, shoulder girdle and upper limbs into the exercise therapy complex, static holding of the limbs (5-7 seconds) in a fixed position, active dynamic exercises for all joints and muscle groups. Assign a massage of the collar zone of the muscles of the back and upper limbs.
Rehabilitation after spinal injuries in the future consists in connecting exercises aimed at increasing the mobility of the spine (tilts, turns of the head and trunk), performed by the patient in the initial position lying and sitting. Exercises are widely used to coordinate movements, to develop a sense of balance, to normalize posture and gait.
Exercise therapy for injuries of the cervical spine during this period can also be carried out in the pool or labor workshops (typing, carpentry and plumbing, pottery, etc.).
Injury of the cervical spine - exercise therapy during the period of traction. Approximate set of exercises
- Diaphragmatic breathing. A load (a bag of sand or a plastic bottle) weighing 1-1.5 kg is placed on the stomach (either in the upper or in the lower part of the abdomen). As you exhale, raise the load as high as possible, hold your breath for 5-10 seconds, lower it while inhaling. It is performed 4-6 times.
- Dorsal and plantar flexion of the feet.
- Squeezing and unclenching the fingers of the hand.
- Circular movements of the feet.
- Flexion and extension of the arms in the elbow joints.
- Alternate bending of the legs in the knee joints, sliding the foot along the plane of the bed.
- Diaphragmatic breathing.
- Flexion and extension of the hands in the wrist joints.
- Alternate abduction and adduction of the legs, without taking them off the plane of the bed.
- Circular movements in the wrist joints.
- Diaphragmatic breathing.
Note. Exercises are performed at a calm pace with pauses for rest. Each movement is repeated no more than 4-6 times. Classes are held 2-3 times during the day.
Additionally, in the complex of physical therapy for injuries of the cervical spine in the period of traction, such labor operations as rolling and rolling bandages and gauze napkins, modeling from plasticine, knitting, etc. are shown.
Injury of the cervical spine - exercise therapy during the period of wearing an orthopedic collar (immobilization). Approximate set of exercises
- Starting position - lying on your back, arms along the body. Flexion and extension of the hands in the wrist joints (6-10 times).
- Starting position - lying on your back, arms along the body. Flexion and extension of the arms in the elbow joints (6-10 times).
- Starting position - lying on your back, arms along the body. Alternate bending of the legs in the knee joints, sliding the foot along the plane of the bed (6-10 times).
- Starting position - lying on your back, arms along the body. Alternate abduction and adduction of the legs, without taking them off the plane of the bed (6-10 times).
- Starting position - lying on your back, arms along the body.
- Starting position - lying on your back, arms along the body. Leading the arm to the side while turning the head in the same direction. Raise your hand - inhale, lower - exhale (4-6 times).
- Starting position - lying on your back, hands on hips. Imitation of cycling (leg movements only alternately!). Repeat 6-8 times.
- Starting position - lying on your stomach. Raising the head and shoulders (6-8 times).
- Starting position - lying on your back, arms along the body. Diaphragmatic breathing (8-10 times).
- Starting position - standing, holding hands on the back of a chair. Rolls from heel to toe (6-8-10 times).
- Starting position - standing, holding hands on the back of a chair. Alternate abduction and adduction of the legs (4-6 times).
- Diaphragmatic breathing (8-10 times).
Isometric exercises for injuries of the cervical spine
- Starting position - lying on your back. Slowly squeeze your fingers with tension for 2-10 seconds (4-6 times).
- Starting position - lying on your back. Slow tension of the back muscles for 2-10 seconds (4-6 times).
- Starting position - lying on your back. Slow tension of the thigh muscles for 2-10 seconds (4-6 times).
- Starting position - sitting on a chair, legs together. Slow tension of the muscles of the chest and abdomen for 2-10 seconds (4-6 times).
- Starting position - sitting on a chair, legs together. Slow tension of the gluteal muscles for 2-10 seconds (4-6 times).
Injury of the cervical spine - exercise therapy after immobilization. Approximate set of exercises
Starting position - lying on your back, arms along the body.
- Diaphragmatic breathing (8-10 times).
- Slowly bend the arms at the elbow joints with tension, bringing the hands to the shoulders (6-8 times).
- Raise the straight leg (by 45º), hold for 5-10 seconds, lower (6-8 times). Starting position - lying on your stomach.
- Hand movements as in breaststroke swimming.
- Alternate abduction of the straight leg back (6-8 times).
- Starting position - lying on your back, arms along the body. Diaphragmatic breathing (8-10 times).
- Hands to shoulders. Raising your hands up, bend in the thoracic spine (4-6 times).
- Circular movement of the arms in the shoulder joints - "mill" (6-8 times in each direction).
- Alternate extension in the knee joint of the leg (6-8 times).
- Starting position - sitting on a chair, legs on a medicine ball. Rolling the medical ball forward, backward, sideways.
- Starting position - lying on your back, arms along the body. Diaphragmatic breathing (8-10 times).
- Alternate abduction and adduction of the legs (8-10 times).
- Half squats (4-6 times).
- Raise your hands up - inhale, return to the starting position - exhale (6-8 times).
Starting position - sitting on a chair.
Starting position - standing, holding hands on the back of a chair.
Note. It is also recommended to include the above isometric exercises in the set of exercise therapy exercises for trauma of the cervical spine after the end of the immobilization period (removal of the fixing bandage).
Spinal injuries can be of a different nature.
Stretching is inherent in the most mobile parts of the spine - the cervical region and the transition region of the thoracic to the lumbar. Stretching occurs during movements of the spine that have crossed the physiological limit of its mobility in a given person. Local stretching is manifested by acute pain, swelling and restriction of movement of the damaged part of the spine due to soreness and reflex contraction of the back muscles. Sprain of the spine is sometimes complicated by paralysis due to concomitant hemorrhage in the spinal cord.
Fractures are exposed to both small parts of the vertebra - the spinous processes, arches, transverse and lateral articular processes, and the body of the vertebra. Fractures of the first kind are partial fractures of a vertebra; fractures of the vertebral body, since they violate the integrity of the spinal column, are at the same time fractures of the spine. Vertebral fractures are the most common.
Fractures of the spine are observed: with gunshot wounds, railway, automobile and other accidents; when falling from a height on the legs, on the buttocks, on the head; with incorrect jumps into the water, etc. In this case, either compression of the spine along the longitudinal axis in combination with flexion, or forced bending of the spine occurs.
Spinal fractures are divided into compression fractures (compression), representing isolated fractures of the vertebral bodies, and fractures with displacement of the spine as a whole. Displaced fractures are also called fractures - dislocations, or luxation fractures (dislocation).
With compression fractures, the spongy bone substance of the vertebral body under the influence of compression along the longitudinal axis is flattened and the vertebra takes a wedge-shaped shape, as a result of which a kyphotic curvature of the spine occurs.
With fractures of the spine with displacement (luxation fractures), a complete transverse or oblique fracture of the vertebral body, ligament rupture, dislocation of the lateral intervertebral joints, and often fractures of the spinous processes and arches occur. The overlying section of the spine is shifted forward and down, moving towards the underlying one; the latter moves back and up and with its posterior edge protrudes into the spinal canal, squeezing or damaging the spinal cord.
The spinal cord in spinal fractures is damaged to varying degrees, ranging from concussions that do not leave visible traces and small hemorrhages that can resolve to a complete transverse rupture of the brain.
Here we will consider only compression fractures and the method of physical therapy for them. The diagnosis of a spinal fracture is established on the basis of clinical symptoms and radiography.
The main clinical symptoms of a spinal fracture are: pain in the area of the fracture, impaired function of the spine and deformity due to a tubercle that forms some protrusion of the spine backwards - kyphosis. An X-ray image will establish not only the presence of a fracture, but also its nature, and most importantly, the position of displaced or damaged vertebrae, which is important for subsequent treatment.
Complications in compression fractures of the spine can be in some cases minor and transient, easily treatable, in others they can deprive the patient of working capacity for many months, difficult to treat. In addition to the above complications from the central nervous system (spinal cord), complications can also affect other organs and systems, such as breathing, digestion, excretion. There are also changes in the psyche in such patients on the basis of exaggerated fear and ashes before the consequences of a fracture of the spine.
Compression fractures of the spine can never be considered only as a local injury to the spine; the echoes of trauma are reflected throughout the body due to the existing cortico-visceral and viscero-cortical connections.
Treatment of uncomplicated compression fractures is carried out in a complex manner and lasts for approximately 3-4 months. Locally, for about one month, the formation of a primary loose callus occurs; within the next month, ossification of the callus occurs, a strong secondary callus is formed, and fragments are consolidated.
In the first period for fractures that are not accompanied by injuries of the spinal cord, physiotherapy exercises are applied 3-4 days after the imposition of traction or a plaster corset, which fixes and unloads the spine well. For fractures accompanied by neurogenic phenomena (paresis and paralysis, disorders of the pelvic organs), exercise therapy is prescribed 2-3 days after the weakening of these phenomena.
General hygienic exercises and exercises for the long muscles of the back are used as physiotherapy exercises - all in the supine position with a very small load. Exercises are used to prepare for an independent turn on the stomach, with a straight back (to preserve the most complete rest of the damaged vertebrae). Excluded are exercises that cause rotations, abduction of the trunk and displacement of the pelvis.
The use of physiotherapy exercises is contraindicated:
1) with fresh fractures subject to surgical treatment;
2) with gunshot fractures in the presence of foreign bodies in the spine;
3) with open fractures with significant defects in the bone tissue;
4) in the presence of complications in the form of inflammation of the bladder (cystitis) during exacerbations and other purulent inflammations of the genitourinary system (uroseptic complications);
5) for fractures in the cervical and upper thoracic spine before immobilization.
Second period begins with the resolution of the turn on the stomach and lasts for 2-2.5 months.
In the second period, the load gradually increases. Exercises for the back muscles are used and exercises are included to create a “muscle corset” (for the abdominal muscles and other muscles of the body). All exercises in traction treatment are performed lying down. By the end of the period, training is carried out to stand up, keeping the spine straight, and training in walking with crutches.
Third period begins with the resolution of walking without crutches.
Exercises are included to increase mobility in the damaged spine from a standing position. The static load on the injured spine increases (carrying small weights on the head). By the end of the period, exercises from a sitting position with a bent lower back are included.
A particular method of physical therapy for spinal injuries without spinal cord injury (according to E.F. Drewing) is determined by the main objectives of treatment and clinical data. In this case, first of all, it is necessary to provide the patient with such conditions under which the restoration of the anatomical integrity of the spine in case of bone damage would occur with the correct direction of the axis of the spine and in the shortest possible time.
For this, the patient is put to bed, as a result of which the spine is unloaded from supporting the gravity of the body. The bed should have a flat surface, for which a thin, tightly knocked together shield and mattress are placed on the bed. The head end of the bed is raised by 15-35 cm, soft straps are threaded under the patient's arms to hold him on an inclined plane in order to easily stretch the fracture area. The straps are attached to the head of the bed. To preserve the natural curves of the spine, small pillows are placed under the cervical and lumbar curves. An ordinary loosely stuffed pillow measuring 40 X 20 cm is placed under the head. The patient's head should be slightly tilted back. In this position of the patient with fractures of the spine, pain sensations calm down.
The patient lies in position only on his back for 8-12 days (in some cases longer). In the future, depending on the nature of the fracture and the general condition of the patient, it is recommended to turn on the stomach. When turning on the stomach, patients should not sit down, since the position with a bent back disrupts proper blood circulation and compresses the affected vertebra.
The patient is taught to turn on his stomach without sitting down, as follows: the patient, lying on his back, moves to the edge of the bed; extends the hand closest to the middle of the bed along the body; with the far hand, he takes the head of the bed, brings his leg to the middle of the bed and turns the torso on his stomach. At first, when turning, you need the help and guidance of a methodologist. In the position on the stomach, the patient is placed under the chest and shoulders (but not under the stomach) with a feather pillow.
From the initial position lying on the back or stomach, patients perform physical exercises for 2 months, starting from the 3rd day after the injury (or somewhat later, depending on the general condition). First, gymnastic exercises of the hygienic type are used 3 times a day for 10-15 minutes; of these, once with a methodologist and 2 times on their own or under the command of one of the patients, the most prepared. In the future, the time of classes gradually increases to 45 minutes, .1 the exercises gradually become more difficult. Before starting the exercises, the rooms are ventilated.
Classes can be carried out individually, but collective (group) exercises are much more valuable and useful, since they have not only a narrow therapeutic value, but also educational, especially for beginners who start classes with some fear and indecision. The methodologist needs to take into account this psychological feature of newly admitted patients, instilling vigor and confidence in them with illustrative examples of other patients. At the same time, it is necessary to monitor patients who show excessive activity and arbitrarily prematurely increase the load, thereby violating the basic law of exercise - the gradual increase in load.
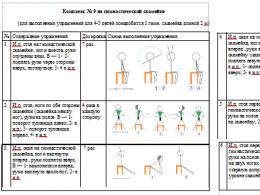
Here is an approximate set of exercises for spinal injuries in the first period.
Classes begin with teaching the patient to complete chest and abdominal breathing (abdominal-thoracic or diaphragmatic). 3-4 breaths are made. The same breathing is used during the moments of the so-called respiratory pauses in the intervals between exercises. Then proceed to gymnastic exercises.
The following exercises are performed
1. Arms extended along the body: clench your fingers into fists and unclench them; the pace is fast; 30 sec.
2. Bend and unbend your arms at the elbows, 5-6 times.
3. Retract and adduct the hands, without taking them off the plane of the bed, 5 times within 4 seconds.
4. Bend and unbend the feet to the back, 10 times.
- Alternately bend your knees, without lifting your hips from the bed, 3-4 times.
- Alternately abduct and adduct the legs in the hip joints, without taking them off the bed.
7. Make a respiratory pause, then 2-3 full breaths.
8. Alternately lower your hands from bed to the floor and raise them to their original position, 2-3 times.
9. Alternately raise your hands to the back of your head, 4-5 times.
10. Legs bent at the knees: bring and spread the knees with slight resistance with the hands, 2-3 times.
11. Make 3-4 full breaths and exhalations.
In total, the exercises will take 15-18 minutes. The complex is designed for 5-6 days when performing exercises 2-3 times a day.
Exercises of the second period are applied from the 8-10th day after the injury, if there are no contraindications to that, until the end of the first month. The complex is compiled with the expectation of involving a large number of muscles in the exercises and a gradual increase
Loads by changing the starting position, range of motion, degree of effort, etc. Exercises should be mostly painless. If, nevertheless, some soreness is noted during individual exercises, the cause of it should be established. With the correct position of the fragments, in the absence of infringement of the nerve roots and other serious clinical phenomena, slight pain during exercise can be tolerated, which usually disappears soon.
In the second period, the following exercises are applied:
- Lying on your back, perform full breathing of the abdominal-thoracic type (individually), 3-4 times.
- Lying on your back, arms are laid apart to shoulder level: simultaneously rotate your arms in the shoulder joints, first forward, then back, for 10 seconds.
- Lying on your back, perform alternate smooth swinging movements with your hands up to the possible limit, 5-6 times.
- Lying on the back, hands behind the head: tilting the head forward and backward with some resistance with the hands and turning the head to the sides, 3-4 times.
5. Lying on your back, arms bent at the elbows: bring your shoulders together (exhale) and spread them (inhale), 5-6 times.
- Lying on your back, holding the bed with your hands: raise the straight leg up within 45 °, bend and unbend the foot, 3-4 times with each leg.
- Bend and unbend in the knee joint alternately each leg, 3-4 times.
- Lying on your back, abduct and adduct each leg in turn, then both legs simultaneously; every exercise is done
9. Lying on your back, arms bent at the elbows, elbows resting on the bed: raise and lower the pelvis, 5-6 times.
10. Lying on the stomach, legs bent at the knees to a right angle: simultaneously bend and unbend the feet to the back at a fast pace, 10 times.
11. Lying on the stomach, arms along the body: tilt the head back, turning it to the sides, 5-6 times.
12. Lying on the stomach, arms on the back, slightly bent at the elbows: fingers are connected in a lock, bend the torso, stretch the arms along the back (inhale) and take the starting position, relaxing the shoulders and back muscles (exhale), 3-4 times.
13. Lying on the stomach, arms bent at the elbows, elbows resting on the bed: raise the pelvis slightly towards the heels and lower it completely, relaxing the back muscles, 3-4 times.
14. Lying on the stomach, arms bent at the elbows: raise the leg up, take it to the side, lead and lower (alternately), 3-4 times.
15. Lying on the stomach, lifting the torso with emphasis on the forearm, 3-4 times.
The whole complex is designed for 30-35 minutes. Exercises are carried out 2 times a day. Between each 2-3 exercises it is necessary to make a respiratory pause.
Exercises for the third period are applied from the second month after the spinal injury. When moving to the exercises of the third period, one should take into account both the general condition of the patient and the degree of assimilation of all previous exercises. The specified period of transition to the exercises of the third period is relative, conditional. The duration of all exercises is 45 minutes.
In the third period, the following exercises are applied:
- Lying on your back, arms along the body: tilt the body to the right and left, sliding the corresponding hand down along the body, and the other hand up to the armpit; leaning to the side to the end, it is recommended to make 2-3 additional slopes in the same direction; the exercise is performed at a slow pace, 3-4 times.
- Lying on your back, turn left and right, 3-4 times.
- Lying on your stomach, raise your torso at an emphasis on outstretched arms and lower it, 3-4 times.
- Lying on your stomach, raise the whole body in emphasis on outstretched arms and lower it, 2-3 times.
- On all fours: stretch the arm forward and the opposite leg back; change arm and leg, trying to maintain balance, 3-4 times.
- On all fours: gradually bend your back and take your head back, then arch your back and lower your head down, 3-4 times.
- On all fours: take a step forward on your knees, then back (alternately with each foot), 5-6 times.
- On all fours: turn your head to the right and look at the right heel; do the same, but in the other direction, 5-6 times.
- On all fours: stretch your arms slightly forward and in this position rock your body up and down, 6-8 times.
10. Lying on your back, hold on to the edges of the bed with your hands: raise both legs by 15-20 cm and lower; then lower your legs down and, without touching the bed, raise them 3-4 times.
11. Lying on your back, raise your right leg and bring it over the left (cross), then the left through the right, 5-6 times.
12. Lying on your back, raise your legs, bend at the knees: make movements with your legs that imitate cycling (smooth alternate bending and straightening of the legs); before the exercise, take a breath, and then make movements for the entire length of the exhalation; as soon as the exhalation is over, take the starting position, inhale and do the exercise again; repeat 3-5 times.
13. Lying on the back, leaning on the forearm, legs bent at the knees: raise the body, arching it upwards, leaning on the back of the head, forearm and feet (“half-bridge”), 3-4 times.
14. Lying on the stomach, hands are laid back, fingers are connected “in the lock”: raise the legs and head (bend), then relax, 3-4 times.
15. Kneeling, hands on hips: turn the torso to the right, take the starting position, then turn the torso to the left, 5-6 times.
16. Kneeling, hands on hips: walk on your knees on the bed.
After every 2-3 exercises, a short rest is necessary.
After two months after the injury, the patient is allowed to get up. Patients are allowed to sit only by the end of the 3rd month, after they learn to walk freely. At first, when sitting on a chair, E.F. Drewing recommends hanging a roller to the back of a chair at the level of the lumbar curve of the spine.
A compression fracture of the spine in children and adults is one of the types of back injury. This injury is characterized by a fracture and damage to one of the vertebrae. This injury is very dangerous, since the damaged vertebra can move into the canal with cerebrospinal fluid and cause paralysis.
When treating this injury, the doctor and his patient must make joint efforts, this is the only way to achieve the desired result, since the restoration of the bone structure takes a long time, and complications can be severe.
A compression fracture with spinal cord injury can lead to lifelong disability.
In what cases is exercise therapy prescribed for damage
Exercise therapy for a compression fracture of the lumbar spine helps the victim restore the flexibility and strength of the spine, and when the spinal cord is ruptured, it helps the patient adapt to his new position with limited abilities. It must be remembered that only specialists should prescribe treatment for spinal injuries, otherwise there may be negative consequences.
It is also necessary to mention that there are a number of contraindications to the appointment of exercise therapy after a compression fracture of the spine:
- Pain syndrome, aggravated during exercise therapy.
- Increased body temperature during and after exercise.
- Drops in blood pressure.
- Deterioration of the general condition in the form of a decrease in sensitivity in the legs and arms.
Important! Physiotherapy exercises should be selected individually for each patient, based on the structure of his body.
Rehabilitation after a compression fracture of the spine of the lumbar spine or another area of it takes a long time - it depends on the degree of damage to the patient's fracture. In childhood, a spinal fracture recovers from 4 to 6 weeks, in middle-aged people this process can take a year, but most often it is five months until the patient is fully restored to work.
Exercise therapy for compression fracture of the spine
There are a number of rules for exercise therapy for spinal fractures that must be followed.
- After an injury, you can not sit for a long time.
- It is allowed to move to a vertical position without a sitting down phase.
- You can only get up from the knee-wrist position.
- Forward bends are prohibited.
- You can't make sudden movements.
- Exercises should be performed carefully, smoothly, as if the patient is in the water.
- Walking is allowed after tests on the back muscles give a positive result.
- Walking should be long, until the appearance of pain at the site of the fracture of the spine.
- The duration of walking gradually increases to 10 km per day.
- It is necessary to evenly distribute the load on the spine while standing, and this can only be achieved with proper posture.
Exercise therapy for a compression fracture of the thoracic spine, as well as the thoracic, is divided into three types:
- Special exercises for stable uncomplicated fractures of the spine without a plaster cast.
- Therapeutic exercise for stable uncomplicated fractures of the spine with walking in a corset.
- Exercise therapy for complex spinal injuries.
If there was damage to the thoracic vertebrae or lower back, the complex of physical culture will consist of four stages.

First stage
Exercise therapy for a fracture of the lumbar spine or thoracic at this stage is prescribed from the first day. The direction of physical therapy in the first period is to restore the body after an injury - improving the patient's well-being, increasing the speed and volume of blood flow, increasing oxygenation by improving respiratory movements and oxygen consumption by cells.
An equally important role in the recovery period is played by the work of the digestive system of the victim, since without sufficient activity of the motility of the stomach, constipation and stagnation can occur, and the lack of nutritional cells quite strongly affects the effectiveness of the entire treatment in the future. A long delay in activity leads to degradation of the epithelium.
Another task of exercise therapy of the first stage is to maintain tone and prevent the development of atrophy of the muscles of the hips, shoulders, and neck. Loss of strength and endurance leads to painful and long rehabilitation, which often ends in disability and loss of all functions of the lower extremities.
Rehabilitation after a fracture of the thoracic or lumbar spine at this stage consists of breathing exercises and a series of exercises that are aimed at developing the strength of small and medium-sized muscle tissues.
Conventionally, exercises for compression fractures of the spine are divided into dynamic static. Dynamic exercise therapy after a fracture of the lumbar spine and other parts of it in this case is carried out in a lightweight version, without muscle overload.

Basically, inhalations and exhalations are practiced, fine motor skills training with the help of tension and relaxation of different muscle groups and raising the legs at a right angle. Much attention is paid to the lower extremity girdle. The loss of muscle mass in the thighs leads to a longer and more difficult rehabilitation in the future, which is limited not only by physiotherapy exercises, but also requires the use of special techniques and equipment.
A set of exercises for the first period:
Breathing exercises:
- In the first three days, perform only diaphragmatic breathing for five minutes 5-6 times a day.
- Starting from the 4th day, the time of breathing exercises is increased to 7 minutes and chest breathing is introduced into the complex, combined with raising the knees in turn and full breathing with increased exhalation.
Gymnastics for the joints is performed 3 times a day for 6 sets with a gradual increase in 12 sets. The following exercises make up the complex:
- Without taking your hands off the bed, gently bend them at the elbows. You can add weights.
- Bending the legs at the knees alternately, and then simultaneously.
- Lifting the lower limb up alternately and together with a gradual increase in amplitude to an angle of 40-45 degrees.
- Retraction of straightened legs to the side.
- Bend your legs at the knees, rest your feet on the bed. In this position, spread your knees to the side.
- Squeeze your fingers and toes.
- Make circular movements with the foot.
- You should slowly strain your fingers for 5-7 seconds.
- Bend your knees while sliding your foot along the bed.
- The patient lies, and slowly strains the oblique muscles of the back for 5-7 seconds.
Gymnastics should be carried out calmly without unnecessary loads with moderate pauses for rest. At the same time, it is important to observe even breathing, all tasks are repeated 5-6 sets several times a day.
Second phase
The second stage takes 4 weeks.
The second period of exercise therapy for a compression fracture of the spine begins a month after the injury and lasts 4 weeks. By this time, the vertebrae are already actively growing together and forming calluses. Exercise therapy in case of spinal injury is due to the formation of an anatomical direction of vertebral growth, which is very important for future rehabilitation.
Breathing exercises, as an independent form of physical therapy, are canceled, but they are included in the gymnastic complex, which must be performed 6 times a day for 25 minutes and the number of approaches: breathing - 3 times, dynamic - 6 times, static - 4 times.
The time of classes increases to 40 minutes, and the number decreases to 4, and the number of repetitions of dynamic exercises increases to 12, and static to 6. At the same time, one new movement is added to the complex daily.
The main goal of the second stage of rehabilitation is the development of a muscular corset of the back, which will subsequently stop the development of additional curvature of the spine and lumbar. A well-timed corset will make it possible to refuse exercise therapy for kyphosis and prevent its possible development due to a violation of the spine.
Exercises are selected for a group of long muscles of the back, transverse short ones, as well as an oblique straight line. All muscles are responsible for the mobility of the vertebrae relative to the axis, which is very important when doing special physical education and subsequent therapy for spinal cord injuries.
The muscle corset effectively affects not only the positive result of treatment after an injury, but is also recommended for maintaining good posture and spinal cord health in healthy people.

It is extremely important to monitor the condition during the session - if pain occurs, you must stop immediately, which will help avoid damage to the spinal cord.
A set of exercises for the second period:
For the starting position - lying on your back with a roller under the lower back:
- Bend your elbows slowly. Put your hands on your shoulders. You need to do the exercise while inhaling.
- On a full exhale, stretch your arms towards the ceiling, and the palms should look at each other.
- Spread your arms to the side as you exhale.
- While inhaling, return the arms to the starting position No. 1.
- Slowly straighten your arms, put them along the body, palms on the bed.
Starting position - lying on your back, legs bent:
- As you inhale, spread your arms out to the sides.
- At the moment of holding your breath, put your hands under your head.
- Make a smooth full exhalation with the simultaneous return of the hands to the position along the body, passing them through the sides. Everything must be done smoothly.
To complicate the exercises, do the leg extension up alternately:
- It is necessary to take the starting position, lying on the stomach with straight arms forward. Your toes should rest on the bed. The coup on the stomach must be performed, observing the technique for fractures.
- When inhaling, tear your forehead off the bed, and strain all the muscles of the body for 7 to 10 seconds. After that, exhale, lowering your forehead to the bed, straightening your feet. Next, you should lie down, completely relaxing all the muscles and breathing calmly for 15 seconds.
Dynamic exercise with two cyclic execution:
- At the same time, while raising your forehead, you should raise the opposite arm and leg. Make 16 smooth movements at an average pace and with a small amplitude. Rest for 10 seconds and then perform 8 more movements, but at a slower pace and with greater amplitude.
- The number of repetitions is from 1 to 4.
Exercise "Scissors" should be performed by increasing the number of movements and the number of approaches, between which it is necessary to pause for rest.
This exercise should be performed lying on your stomach, with your hands under your forehead, only after the permission of the doctor. And before that, it is necessary to lie with your arms along the body and your head, which is first turned to one side and then returned to the other side.
Third stage
The third stage begins approximately 50-60 days after the injury.
It takes two months to start the third stage of treatment. Exercises against the curvature of the upper spine become more frequent and longer. If the victim can support his body and back with a compression fracture of the lumbar spine vertically without outside help, then you should move on to light walks and back warm-ups, which quickly give a positive therapeutic effect.

Period 3 - the load increases, the therapeutic effect increases due to a set of exercises with resistance, weights and isometric uniform exercises that contribute to the development of muscle corset tone. If at this stage the victim already has formed back muscle groups, the treatment is much faster and easier.
The transition to a new load package should be gradual. The exercise therapy specialist introduces new types of exercises that were not previously available to the patient. The starting position of this complex is on your knees and on all fours. Swings, movements of arms, legs, deflections in this position have a very beneficial effect on the spine.
A set of exercises of the third stage:
- Tilts back, forward.
- Tilts to each side or left, right.
- Walking back and forth on your knees.
- Crawl on all fours left and right.
- Tilts back.
- Flexion of the elbow joint with a weighting agent up to 2-3 kg.
- Diaphragmatic breathing.
All of the above exercises must be performed in 6 sets, at least twice a day. The duration of one exercise should not exceed 20 seconds.
The main tasks of exercise therapy at this stage of therapy are to prevent the development of posture disorders, increase the reactivity of the whole organism and completely restore all functions of the spine.
Fourth stage
It begins after the patient gets out of bed on his own. The timing of this period depends on the effectiveness of exercise therapy and the severity of the damage. At the fourth stage, the specialist begins gymnastics with kyphosis or lordosis. These pathologies developed in the patient immediately upon rupture, with a fracture of the spine.
It is advisable to carry out exercises for kyphosis of the thoracic spine in this period in the conditions of an exercise therapy room - otherwise the patient may not have enough space and equipment. It is allowed to replace many special devices with auxiliary ones. For example - a gymnastic rack on the windowsill.
The fourth stage is allowed, with a number of exceptions, to take place at home. But it is important that the care is carried out properly. Weight lifting, jumping, fast running are absolutely unacceptable - this can provoke damage to newly fused vertebrae. If possible, it is advisable to stay in a rehabilitation center, especially if the victim lives far from him and does not have the opportunity to visit a surgeon or traumatologist.

A set of exercises of the fourth period:
- Within 7 seconds, strain the muscle tissue.
- Make small translational movements of the pelvis forward, backward.
- Rolling from toe to heel do 8 times.
- Tighten the muscles of the buttocks for 7 seconds.
- Starting position - the back is straightened. Do semi-squats on toes - inhale, the starting position is exhale.
- Pull back the leg with resistance.
- Tighten the muscle tissue of the thighs for seven seconds.
- Passive rest.
Also at this stage, it is possible to carry out massage in case of a fracture of the thoracic vertebrae and its other zones. The classic type of massage and acupressure are used. Massage improves blood circulation and metabolism in the body.
Massage must be performed smoothly, in stages without haste.
For each patient, the doctor makes an individual rehabilitation complex, which includes:
- Physiotherapy procedures.
- Walks, including dosed walking, health path, therapeutic walking on the stairs or on the step platform.
- Exercises that can be done in the gym.
- Scheme of training in dosed swimming.
The benefits of physical therapy
The purpose of therapeutic exercises depends entirely on the degree of injury. With a compression fracture, the course of treatment is on average one year. Special physical education is able to return to the patient all the anatomical functions of the spine and excellent health without discomfort in one year.
Exercise therapy will help to stop all the negative consequences after the violations of muscle activity that have occurred. It also helps to stabilize various nervous processes, and also normalizes the work of various systems in the body after a long lying down. Increases the rate of regeneration of damaged bones of the spinal column. Exercise therapy has a complex effect on the body as a whole, eliminating negative consequences.
Do not delay with the diagnosis and treatment of the disease!
Sign up for an examination with a doctor!
Any injuries associated with the spine are the most severe injuries of the musculoskeletal system. Of great importance is exercise therapy for spinal injuries.
A set of classes in such cases is prescribed exclusively by a doctor and is carried out taking into account the stage, as well as the type of pathological process.
The value of physiotherapy exercises for spinal injury
Through the use of physical therapies:
- the process of blood circulation improves, as a result of which the resorption of hematomas and destructive tissues increases;
- there is an acceleration of the regeneration of nerve fibers;
- muscle tone is normalized;
- metabolic and energy processes are improved;
- the feeling of pain decreases;
- the body's defenses are activated.
When can I start physical therapy after a spinal injury?
First of all, these are general prevention exercises that are aimed at preventing the development of bedsores, as well as congestion in the lungs. The process of treatment of spinal injuries is carried out strictly in stages, each stage corresponds to a certain set of classes.
Therapeutic exercise in the presence of spinal injuries
The most elementary complex of physiotherapy exercises is performed in the initial position lying on your back with outstretched arms along the body and consists of the following exercises:
- Spread your arms to the sides when inhaling, and as you exhale, stretch them forward, and then lower them down (three to four times).
- Bend slowly, but with tension in the arms in the elbow joints, while bringing the hands to the shoulders (from four to six times).
- Perform six to ten times plantar and dorsiflexion of the feet.
- Move your hands to the side while turning your head in the same direction. Repeat the exercise now on the other side (four to six times).
- Bend your leg at the knee joint, pull it up, then lower it. Do this eight times.
- Diaphragmatic breathing five times.
- Put your hands on your hips and pretend to ride a bike. Do this exercise eight times with each leg.
Gymnastics
A spinal fracture is a violation of the integrity of the bones related to the spinal column. Such an injury requires a long recovery, the joint efforts of the doctor and the patient. It can be of different types: from compression - to damage with a rupture of the spinal cord, in which a person remains disabled. In the first case, physical therapy is designed to return the patient to his former mobility, in the second - to adapt him to life with disabilities.
The role of exercise therapy in spinal injury
The tasks of exercise therapy depend on the severity of the injury. With a compression fracture, the duration of the course is about a year. During this time, the patient fully returns to its former mobility and good health. With a fracture complicated by an incomplete rupture of the spinal cord, rehabilitation takes much longer, and its goal is to fully restore health. With injuries accompanied by a complete brain rupture, special exercises are designed to teach a person to live in conditions of limited ability to work.
Therapeutic exercise has a stimulating and tonic effect on the patient's body. It eliminates the negative effects of physical inactivity, contributes to the normalization of nervous processes, improves the functioning of other organs and systems, in particular, respiratory and cardiovascular.
Special exercises activate the body's defenses, prevent the appearance of various complications provoked by a long stay in one lying position.
Exercise therapy activates metabolism, prevents the development of muscle atrophy, accelerates regeneration processes in the damaged area of the spine. It has a compensatory effect, helping to strengthen the muscles of the body as much as possible, develop a muscular corset capable of holding the spinal column in the correct position, and thereby neutralize the insufficient endurance of its damaged area.
Physical exercise is an essential element of post-traumatic rehabilitation. They allow you to restore the normal mobility of the spine, its support and shape.
Exercise therapy is prescribed in the first days of the treatment process, when contraindications due to the general manifestations of a traumatic disease are eliminated.
With a compression fracture, exercises are indicated to the patient when his condition meets the following criteria:
- body temperature returned to normal;
- the skeleton is compared, elements of osteosynthesis are removed: gypsum, knitting needles, wires, etc.;
- The doctor performed a control X-ray and noted the positive results of therapy.
The duration of the recovery process depends on the severity of the injury and the age of the patient. In children with compression fractures, the rehabilitation period is 30-40 days, in adults it stretches for a longer period. Usually 4-5 months are enough to fully restore the victim's ability to work.
For the prevention and treatment of DISEASES OF THE JOINTS, our regular reader uses the method of non-surgical treatment, which is gaining popularity, recommended by leading German and Israeli orthopedists. After carefully reviewing it, we decided to offer it to your attention.

Exercise therapy is the basis of functional therapy. It is the special gymnastics, selected individually for the patient by his attending physician, that helps to finally restore mobility and flexibility. It strengthens the muscles of the chest and lumbar, shoulder girdle and pelvis.
When treating a patient with a spinal fracture with motor activity, it is advisable to adhere to the generally accepted division of exercise therapy into three periods.
First period of therapy
This is the earliest period, it includes exercises that are carried out within a month after receiving a spinal injury. This stage includes careful movements of the limbs, as well as various types of breathing activities.
Doctors recommend the following exercises:
- diaphragmatic breathing;
- rotation of the feet and hands;
- finger flexion;
- flexion of the legs at the knee joint;
- abduction of the lower limbs to the side.
Therapeutic gymnastics of the first period includes one important rule: when performing activities, the patient should not tear off the limbs from the bed. This prevents the possibility of straining the muscles of the pelvis and shoulder girdle, which minimizes the likelihood of displacement of the vertebrae and other side effects.
Physical education of the first stage lasts 6-12 days. The patient performs exercises independently twice a day. The recommended duration of "charging" is 10-15 minutes. The first lessons with the patient should be conducted by a methodologist-instructor, then it is possible to unite the victims into groups.
The principle of building classes at the first stage is as follows: at the beginning, the patient is recommended lighter gymnastics, then more complex activities are included in the class. A strong load is not given to the pelvic girdle, but the muscles of the shoulders are actively involved in the work. Gradually, careful training of the muscles responsible for back extension begins.
On the 8th-14th day after receiving a compression injury, the patient is shown turning on his stomach. They are performed as follows: a person rolls up to the edge of the bed, holds on to its headboard with one hand, and with the help of the other carefully rolls over. The first exercises of this kind should be carried out in the presence of a methodologist.
The recommended duration of the first stage is until the end of the first month of a person's stay in bed after a spinal fracture. Further, if the person feels well and there are no contraindications, the transition to the second stage is carried out.
Exercise therapy in the second period of treatment
The second stage of functional therapy begins from the second month of treatment. The intensity of classes increases: the number of repetitions and the amplitude of movements increase. The main task of this period is to strengthen the muscular corset. The duration of the "charging" increases first to 20, and then to 45 minutes.
The patient performs the following exercises in the supine position:
- breeding to the sides of the hands;
- touching the hands of the shoulders;
- muscle tension in the thigh area;
- "bike";
- alternate lifting of the lower extremities to an angle of 45 degrees.
The patient is shown gymnastics at least twice a day in an organized group. Also, the patient should practice independently at least twice a day. The second period is aimed at training flexibility, as well as the development of the extensors of the back. The muscles of the pelvis, thoracic and lumbar spine are connected to the classes.

Therapeutic exercise should be done independently at home after discharge from the hospital
For moderate fractures, the patient is allowed to get out of bed after 60 days of treatment. During the lifting process, the patient should not sit down. To get on his feet, he uses the following technique: he gets on all fours, crawls to the edge of the bed, and then alternately lowers both lower limbs to the floor.
Allowing the patient to stand up, the doctor should be guided by the following signs:
- the person has no pain in the area of the injured spine;
- no discomfort when tapping damaged vertebrae;
- lack of protrusion at the fracture site;
- good health after class.
When the patient first got out of bed, therapeutic exercises of the third period can begin.
Exercise therapy of the third stage
The duration of the third period is at least two months. At this stage, the patient is recommended more intense physical education, including activities with resistance and weights. The muscles of the pelvis, legs, and lumbar are connected.
The most commonly used exercises are:
- lifting the shoulders and head lying on the stomach;
- abduction of legs tied with a rubber band;
- movement in a pose on all fours;
- body tilts to the sides from a standing position.
At first, the patient is allowed to get up no more than 3-4 times a day for only 20-15 minutes. Gradually, the duration of classes increases. By the end of the third month of functional therapy, the patient should be able to walk for 1.5-2 hours without rest.
Only after a person has learned to walk for at least an hour can he sit. It is important to maintain correct posture: for this, a round roller is hung on the chair where the patient will be located at the level of the lower back.
Therapeutic gymnastics is an essential condition for recovery. It is mandatory to carry out during the patient's stay in the hospital, it should be done independently at home after discharge. Only regular "charging" will allow you to quickly recover from an injury and restore the former flexibility and mobility of the spine.